Thyroid & Parathyroid Surgery in Atlanta
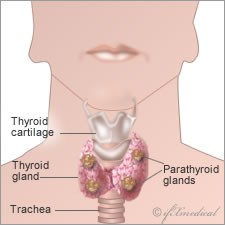 While all surgeries can be intimidating to those who need them, thyroid and parathyroid surgeries are extremely common surgeries, largely due to the wide range of conditions that call for them.
While all surgeries can be intimidating to those who need them, thyroid and parathyroid surgeries are extremely common surgeries, largely due to the wide range of conditions that call for them.
Thyroid surgery, for instance, is commonly required to treat nodules, enlarged thyroid glands, cancer, and over-active thyroid glands. Parathyroid surgery is often the prescribed treatment for hyperparathyroidism or overactive parathyroid glands.
Thyroid Surgery
Thyroid surgery generally requires anesthesia. Some surgeons prefer light sedation and local anesthesia so that patients are awake during the surgery, but for the most part full anesthesia offers more options in the operating room.
A total thyroidectomy involves the removal of the entire gland while a subtotal or partial thyroidectomy removes only part of the thyroid gland.
Patients undergoing thyroid surgery are generally admitted to the hospital the day of the surgery and either released the night of the surgery or the morning after if there are no complications.
Thyroid Surgery Risks
All surgeries carry risks of bleeding and infection. Thyroid surgery carries the additional risk of nerve injury and a need for thyroid and/or calcium replacement medication, as well as a failure to diagnose cancer at the time of the surgery (resulting in the need for additional surgery), and hoarseness.
Parathyroid Surgery
Patients who need parathyroid surgery have the option of Minimally Invasive Radioguided Parathyroidectomy (MIRP). This surgery involves the use of sestamibi radioactive markers that surgeons can follow with a handheld probe so that they are able to minimize the exploratory aspect of a traditional parathyroid surgery. This particular treatment typically takes less than one hour to complete and patients can return home within a few hours of the procedure.
Patients who have multiple-gland disease or have negative sestamibi scans will generally undergo an intraoperative parathyroid hormone blood test (IOPTH) in order to confirm that all abnormal tissue has been removed.
Parathyroid Surgery Risks
Hoarseness is a common side effect as is the need for thyroid placement. Calcium replacement therapy may be required and in rare cases, may be a lifelong occurrence. Permanent hoarseness is extremely rare, but is a possibility.
After the Surgery
Because calcium deficiencies are so common in the aftermath of thyroid and parathyroid surgeries, your blood calcium levels will be closely monitored after the surgery (before leaving the hospital and at follow-up visits with your physician).
You will have the surgical bandage removed and replaced with a waterproof bandage before being released and are free to talk, eat, and drink once you awaken. You will have a follow up visit within a week of your surgery to track progress, examine the wound, adjust medications, and remove sutures if necessary.